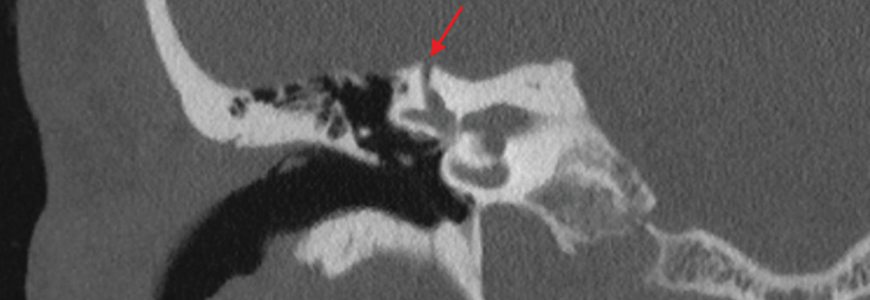
Superior semicircular canal dehiscence (SSCD), a hole in or thinning of bone in the inner ear, occurs in approximately 1 to 2 percent of people. Of that small group, a much smaller number of people will experience symptoms of semicircular canal dehiscence syndrome (SCDS). Doctors within Duke Health’s Head Neck Surgery & Communication Sciences Department are experts in the diagnosis and treatment of this debilitating syndrome.
Common symptoms of SCDS include sound-or pressure-induced episodes of brief dizziness or vertigo, bone conduction hyperacusis, and autophony. Even with a clear set of diagnostic criteria, making this diagnosis is challenging, according to Eric J. Formeister, MD, MS, a head and neck surgeon who specializes in neurotology at Duke Health. This is especially true because nearly half of people with SCDS experience overlapping symptoms with co-occurring vestibular migraine.
The need for careful and cautious diagnosis is one reason why Dr. Formeister recommends physicians consider a specialist referral for any patient who has unclear symptoms.
To refer to Duke, call 1-800-MED-DUKE (800-633-3853) or log into Duke MedLink.
“Specifically for superior canal dehiscence syndrome I understand the symptoms and frustration of chronic dizziness syndromes like this one and want to match people with the best treatment course for them,” he says. “Some people may not end up needing surgery, but they will get treatment or a referral to someone who can help if they come to us for treatment.”
When surgical intervention is necessary, different approaches may be warranted based on a patient’s unique situation and anatomy. The typical transmastoid approach can achieve symptom relief for some. Others may benefit more from an image-guided middle-fossa craniotomy approach, which allows for a smaller craniotomy.
However, Dr. Formeister also wants to be clear: Craniotomy, even if the size of a keyhole, is not minimally invasive surgery.
Given the risks that accompany procedures to treat SCDS, which, though rare, include deafness or profound balance loss, it is crucial for patients with SCDS or suspected SCDS to consult a program with significant experience diagnosing and treating it. Surgeons at Duke Health, including Dr. Formeister, are well-experienced in this area. He himself trained with one of the world’s experts in this condition, and as a result has performed more than 130 SCDS surgeries to date.
After surgery, Duke’s Health’s unmatched expertise managing all types of skull-based surgical conditions means the post-surgical staff also know how to care for the unique challenges and needs of patients who have undergone SCDS surgery. Dr. Formeister specifically cites the importance of inpatient vestibular physical therapists as a unique benefit of having this surgical procedure at Duke Health, as rehabilitation is quicker and more effective when guided by physical therapists just after the surgery. The full spectrum of expertise in caring for these conditions can be the key to ensuring the best possible outcome for people living with SCDS.