Expansion of “Off-Label” TAVR Highlights Potential for Accelerated High-Risk Device Use in United States
The expansion in the use of “off-label” transcatheter aortic valve replacement (TAVR) reflects the potential of accelerated, safe high-risk device use in the United States as stakeholders from across the “device ecosystem” begin to streamline regulations, says Robert M. Califf, MD, MACC, former chief of the US Food and Drug Administration (FDA) and current vice chancellor for Health Data Science at Duke.
In an editorial published in JAMA Cardiology, Califf suggests that “off-label” TAVR use with a high-quality registry to measure outcomes has contributed to regulatory reform.
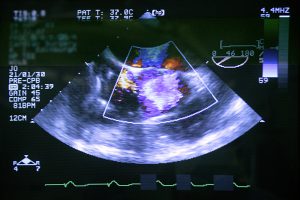
Califf’s editorial appears alongside an analysis prepared by the National Cardiovascular Data Registry comparing outcomes of patients who underwent TAVR “on-label” vs those who did so “off-label.” The majority of the patients treated “off-label” had significant aortic or mitral valve regurgitation that raised concerns about the technical performance of the procedure.
But, after adjusting for differences in patient, clinical, and facility characteristics, Califf writes, “the differences in major cardiovascular outcomes were not statistically significant.”
When TAVR was first developed, an estimated 4.5-year delay between European and United States access to the procedure “crystallized concerns that early device development was stymied in the United States by regulatory barriers,” Califf writes, denying patients access to “useful, even life-saving devices.”
As a result, changes are underway. The FDA, the Centers for Medicare and Medicaid Services (CMS), expert clinicians, and leaders in the medical device industry have revamped the system of early device development, including the clinical-trial and FDA-review processes. An Early Feasibility Studies program has brought stakeholders together who have suggested several key improvements:
- Streamlining institutional bureaucracy (eg, institutional review boards, contracting, and liability issues in leading cardiology interventional centers)
- Enhancing clinical research performance
- Accelerating FDA and CMS review
- Improving timeliness for reimbursement and funding
To continue the expansion, Califf argues that device development should begin with the most obvious clinical indication in which the risk–benefit balance is most favorable. Expanded indications will be supported by national registries and randomized trials using electronic health records and other data sources.
With such an approach, inventors and manufacturers will see reductions in development and evaluation costs, and clinicians, the FDA, and CMS will have higher-quality evidence to inform decision making at the individual and population levels. Most importantly, Califf emphasizes, patients will have confidence they are receiving beneficial device procedures in the context of high-quality clinical care.