The Duke Electrophysiology (EP) team has emerged as a regional and national referral center for pacemaker and defibrillator lead extraction by building a long-term record of safe removal, particularly for patients with complex presentations.
The EP team performed 120 lead extractions in 2019—the highest total in program history and highest in the southeastern United States—and is among the highest volume centers in the nation. The team announced two expansions this summer: at WakeMed Health and Hospitals in Raleigh, NC, and the Durham Veterans Affairs Medical Center in Durham, NC.
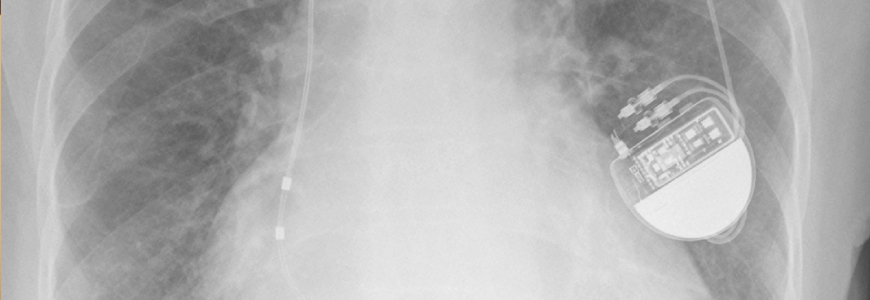
Approximately 3 million patients in the United States have a pacemaker or defibrillator and approximately 12,000 undergo lead extraction procedures each year, many for infection of the device, says Robert K. Lewis, MD, PhD, director of Duke’s lead extraction program.
Pacemaker and defibrillator infections can have serious consequences if not managed appropriately. Because of the risk associated with complex lead removal, many physicians used antibiotics to treat infections, typically without success. But the Duke extraction team, which includes Donald D. Hegland, MD, Sean Pokorney, MD, MBA, and Jonathan P. Piccini Sr., MD, MHSc, has demonstrated that removal is a preferred option.
Other than infection, leads are often removed due to malfunction. Removing dysfunctional or infected leads is a challenging procedure, cardiologists say, because scar tissue develops making them difficult to extract without risking tears or punctures in heart tissue, which could then introduce the potential for catastrophic results.
Extractions require hybrid operating rooms with high-grade fluoroscopy
“The skill level of these practitioners is critically important,” says Manesh R. Patel, MD, chief of the Cardiology and Clinical Pharmacology divisions at Duke Heart. “But lead extractions done by highly skilled electrophysiologists have become very safe with good outcomes. This team has achieved an impressive safety record.”
The Duke electrophysiologists partner with cardiothoracic surgeons and anesthesiologists during surgical removal procedures to prepare for any outcome, Lewis says. The extractions are performed in hybrid operating rooms equipped with high-grade fluoroscopy for improved imaging.
“The pace of growth is based on our clinical reputation,” says Lewis. “We make it possible to perform lead removal for patients who have been turned away otherwise because the procedure was considered too risky to undertake.”
Another contributor to referral growth is increasing awareness that safe extraction is possible. In the past, dysfunctional leads were frequently replaced with another one to avoid the risk of removal. That trend is now changing, Lewis says.
“Referring cardiologists are seeing our results, even in complex cases; we have set an industry standard for safety and good outcomes, and they are comfortable with our approach,” Lewis says. “We make it possible to perform lead removal for patients who have been told it’s not possible. We resolve the lead issue and send the patient back to the care of the referring practice.”