At Duke Health, comprehensive care for head and neck cancer includes more than just a full suite of treatment options to address the cancer itself. Allied health services such as speech pathology, physical therapy and nutrition are integrated into the care plan as early as possible for every patient, often even before a treatment like radiation, surgery or chemotherapy begins. The goal is to ensure that people recover as quickly and fully as possible, so they can successfully return to daily life.
“Early intervention is important, especially for patients who expect to have bilateral radiation of the neck,” says Mindi Ramsey, M.A., CCC-SLP, a senior speech-language pathologist at Duke Voice Care Center, which is imbedded in the Department of Head and Neck Cancer and Communication Sciences. “We really try to evaluate them right after diagnosis to establish a baseline of their function before treatment starts.”
These evaluations are also a valuable opportunity for therapists to educate the patient about what to expect in terms of post-therapy side effects and to offer them recommendations ahead of time for activities that may preserve critical functions like swallowing.
Research has shown that people who actively use muscles for activities like eating or exercising have better swallowing outcomes 5 years after radiation therapy for neck cancer. So, after cancer treatment starts, the embedded therapists follow up in short order to get the person to start re-using muscles critical for swallowing or speech. This might mean arranging post-operative inpatient therapy visits or making a coordinated plan to see them during their first outpatient follow-up appointment. The embedded team at Duke also offers specialized therapies that aren’t always available in speech clinics, such as manual therapy for the mouth, throat and neck, which Ramsey says has been integral to improving range of motion for speaking and swallowing in her patients.
Integration with the clinical head and neck cancer specialists is crucial to recovery success. Within the head and neck cancer program, the therapists work side-by-side in the same clinic as oncologists and surgeons. When possible, they see people on the same day as their outpatient medical or surgical appointments.
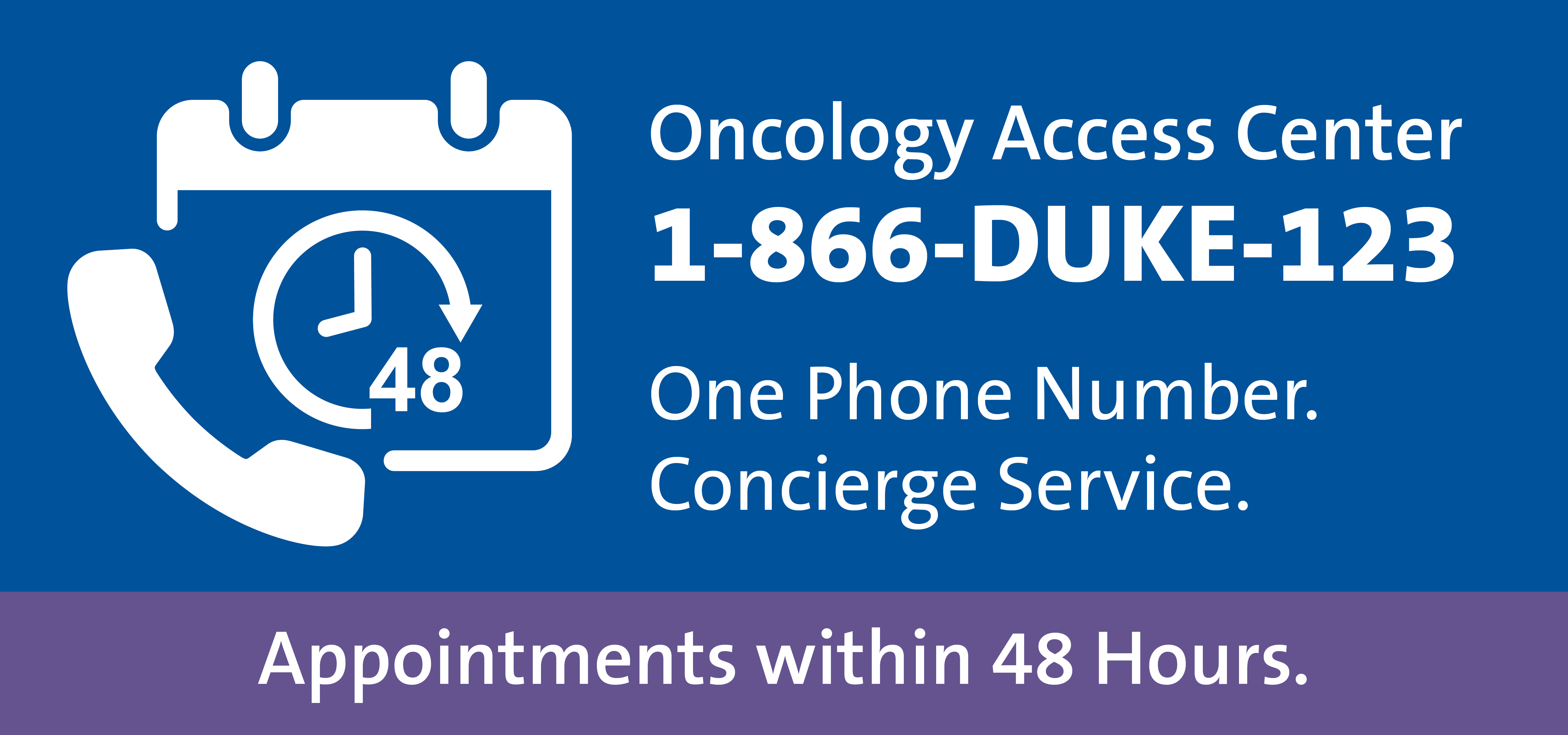
Our referring provider team makes referring patients to Duke Cancer Centers efficient and easy. Call Monday through Friday, between 8 a.m. and 4:30 pm.
You can also email OncologyReferral@Duke.edu or use the referral form below.
The entire team—medical and surgical oncology, nurses, therapists and others involved in the care plan—meet regularly to discuss every aspect of treatment progress. The week-by-week view that the therapists have provides everyone with a better sense of the patient’s trajectory. “We see what the day to day is like for that person who is living with cancer or the side effects of its treatment,” adds Ramsey. “We are very proactive about communicating symptom changes so we can all collaborate on how to treat them best.”
The team brings in other specialists as needed such as medical dental specialists, physical therapists or counselors to tackle any barriers to recovery. Ramsey says that the team’s specialized training and expertise dealing with a wide variety of impacts from head and neck cancer and cancer therapies, coupled with their focus on the full spectrum of recovery, is what makes Duke Health’s head and neck cancer care top notch.
The speech pathologists and other support services are a part of that picture. “These issues are critical to their healing process and enhancing their quality of life,” Ramsey concludes. “And that’s our collective goal.”
