A renal pathologist with international research experience has joined Duke Nephrology to help leverage emerging digital imaging and artificial intelligence (AI) technologies that now influence pathological imaging and interpretation.
Laura Barisoni, MD, who will become president of the Renal Pathology Society in 2019, will strengthen Duke’s partnerships with National Institutes of Health (NIH) research consortia such as the Kidney Precision Medicine Program, the Nephrotic Syndrome Study Network (NEPTUNE), and the Cure Glomerulonephropathy (CureGN).
By emphasizing the latest imaging technologies and applying AI as an analytical tool, Barisoni plans to accelerate the work of the well-established Duke renal pathology team in expanding precision medicine diagnostic capabilities.
“Computer-aided image analysis is not meant to be a substitute for the work of pathologists,” says Barisoni. “The objective of the technology is to enhance the work of the pathology team by using computational power to enable more precise interpretation of biopsy imaging.”
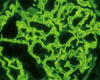
Duke renal pathologists want to provide more quantitative data than has been possible through visual interpretive methodologies. Newer, more innovative technologies can be used to score and assess biopsies. AI technologies and computational power can manage the time-consuming and sometimes challenging processes of counting cells in tissue samples, for example.
“It’s almost impossible for a pathologist to count cells in a biopsy, and even when it can be done, the process is incredibly time consuming,” she says. “Computational technology uses AI and pattern recognition to count every inflammatory cell, all the tubules, and all the glomeruli to yield quantitative data. Now we have a more accurate, more quantitative assessment.” In addition to cell counts, the technology can measure the density of interstitial fibrosis and identify or highlight structures that a pathologist should evaluate.
Several international research consortia, Barisoni says, are collaborating to implement standardized pre-analytic, analytic, and post-analytic phases of the digital pathology analysis, paving the way for novel models of integrated pathology and fused diagnostics.
The application of AI for visual and subvisual structural feature extraction from kidney tissue, paired with complementary information from clinical and molecular profiles, will enable more clinically meaningful patient categorization. Thus, the creation of permanent digital pathology repositories of renal biopsies opens the door for Duke to enhance the role of pathomics in advancing the diagnosis and treatment of kidney disease.
In conjunction with Barisoni’s arrival, Duke Nephrology will become an enrolling site for the third phase of NEPTUNE, the well-established consortium for comprehensive characterization of patients with nephrotic syndrome. In alignment with the Duke mission of implementing precision medicine, patient-specific morphologic and molecular profiles captured with the NEPTUNE protocol will provide information to guide more targeted therapies.