Now in its fourth year, the Duke Primary Care Depression Initiative (DPC-DI) has reached more than 1,000 patients, significantly improving outcomes and patient satisfaction. The evidence-based, collaborative care program, which integrates depression care management into primary care, is now available in all 27 Duke primary care clinics.
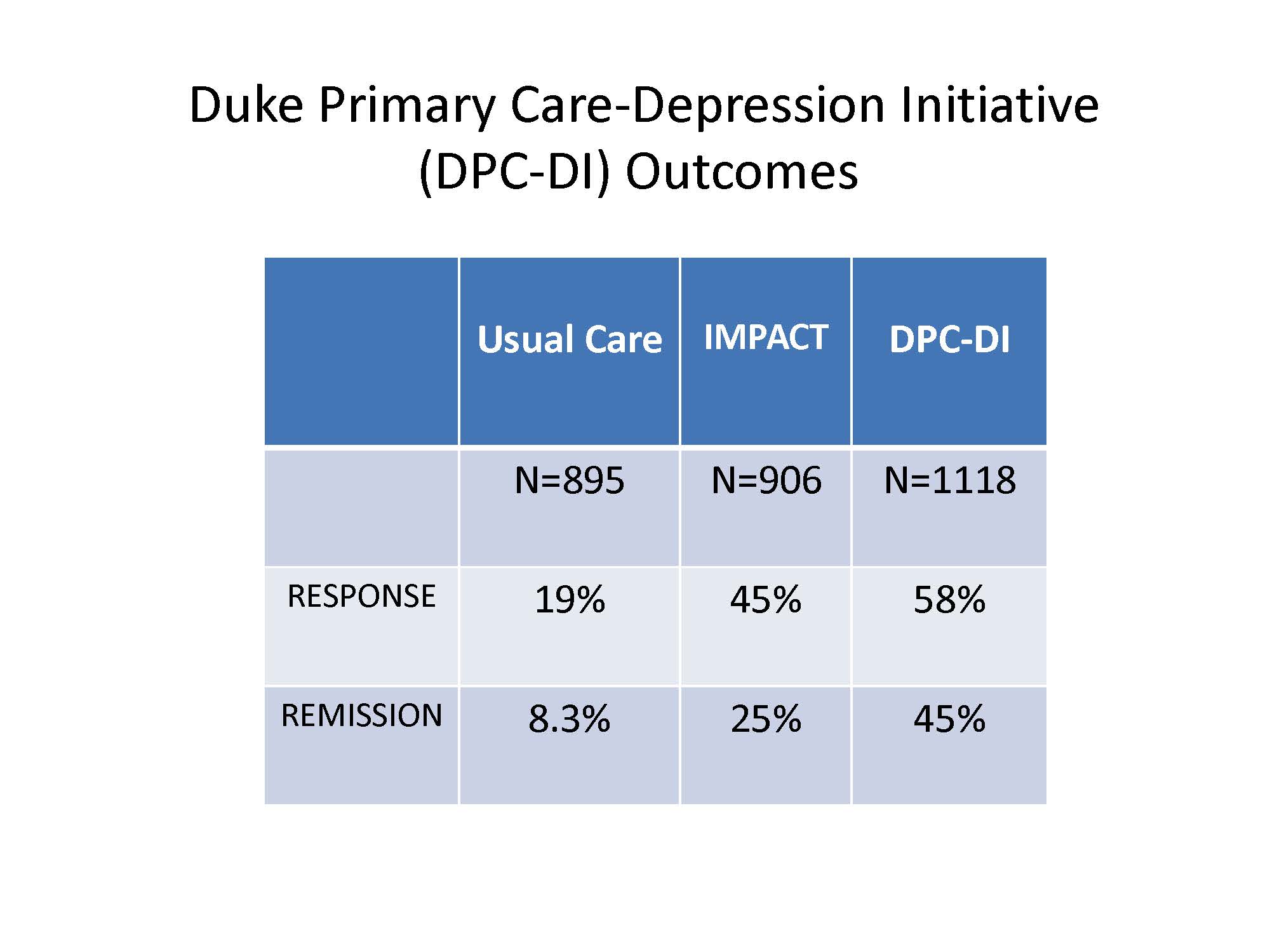
DPC-DI’s structure is modeled on the University of Washington’s Improving Mood—Promoting Access to Collaborative Treatment (IMPACT) study, the first large, randomized control trial of a collaborative care model for depression. The study showed that the model was more than twice as effective as traditional depression care for older adults in primary care settings. The findings have since been replicated in more than 80 randomized clinical trials.
Like the original IMPACT care model, DPC-DI involves the incorporation of a team of psychiatrists and care managers into the standard PCP–patient relationship. Unlike the original model which treated patients 65 and older, the Duke program treats adults over 18 years of age.
The process starts at the primary care clinic where patients are screened with the PHQ-2 at their yearly visits or if there is concern for depression. Those who screen positive are further evaluated with the full PHQ-9 to determine whether they meet the criteria for depressive disorder. Patients who score a 10 or above on the scale are referred for depression care management, comprising an initial phone call with a care manager, who performs follow-up screening and obtains additional relevant information.
The care manager meets weekly with the psychiatry consultant to review each patient’s results and determine the best course of action. Recommendations are then sent back to the PCP via EHR, so the PCP can implement the plan as appropriate.
“To me, one of the most rewarding things about this approach is that it is breaking down barriers to care for patients—stigma, transportation, cost—and bringing them evidence-based care in a timely manner.” says Virginia O’Brien, MD, medical director of the initiative.
Feedback from physicians show that satisfaction with the Duke program has been high, she says, and, despite being entirely telephonic, DPC-DI’s outcomes exceed those of the original IMPACT model. Following participation in the program, 58 percent of patients had a response and 45 percent went into remission—defined as a 50 percent or greater reduction in their PHQ-9 score and a score of less than 5, respectively.
An important component of the initiative’s success has been the strong relationship between Duke Psychiatry and the primary care clinics, O’Brien says. To truly be successful, research shows that these types of depression treatment programs must be truly collaborative.
“Some places offer co-located care or telemedicine,” she says. “That’s fine, but there’s not a lot of evidence showing that these approaches confer a benefit for mental health conditions. This initiative is exciting because it brings together people from a variety of areas in healthcare who collaborate to provide the best possible care for patients in our community. That, to me, is what medicine was meant to do.”