A 14-year-old female patient presented to Muhammad Zafar, MD, pediatric epileptologist at Duke Children’s, with frequent seizures before and during sleep. Her seizure onset began at two months of age with infantile spasms. Seizures initially resolved after adrenocorticotropic hormone (ACTH) therapy but came back eight years later occurring six to seven times per night with impaired awareness.
An electroencephalogram (EEG) indicated that seizures were originating from the right side of the brain. Initially, an MRI and PET scan showed no abnormalities. However, upon further review by an epilepsy neuroradiologist, a potential seizure focus was identified in the right frontal lobe. Since this area is near the area of the brain that controls movement in the arm and leg, surgical resection was not considered at that time.
Zafar continued to monitor the patient capturing numerous right frontal seizures on EEG. As a teenager, the patient’s seizures were severely impacting her quality of life and ability to engage in normal activities. Phase two invasive monitoring was initiated to learn more about where the seizures began. This involved stereotactically placing depth electrodes with robotic assistance (Stereo EEG) for EEG recording. Bedside mapping was also performed to localize the motor area of the brain and to assess the patient's eligibility for surgical resection.
Results showed that the areas of the brain requiring removal to treat the patient’s seizures were very close to the area of the brain that controlled her left hand. Zafar then consulted Duke pediatric neurosurgeon and Chair of Neurosurgery, Gerald A. Grant, MD, to advise on a recommended procedure.
“We closely followed this patient for several years and went back and forth on doing the surgery because of the potential complications. The patient even went to another major medical institution for a second opinion, but the parents were hesitant. Dr. Grant and I collaborated to give her an option that the parents felt comfortable about,” says Zafar.
Question: What innovative surgical option did Zafar and Grant offer this patient and her family?
Answer: Zafar and Grant developed a plan for precise resection of the abnormal area of the brain causing the seizures using EEG directly on the brain in the operating room. First, Grant performed a craniotomy to place electrodes on the brain’s surface to record electrical activity from the cerebral cortex. With EEG, Zafar could monitor the patient’s brain signals.
“The risks were high because the patient could have become paralyzed and still have seizures,” says Zafar. “Dr. Grant, however, was confident in his abilities to achieve an excellent result with detailed mapping of her left arm and leg during surgery, and that earned the family’s confidence too.”
EEG allowed Grant to very precisely resect only the affected areas of the patient’s brain—nothing more.
The patient tolerated the procedure well. One-year post-op, she remains seizure-free with no deficits. “Now, she’s doing the normal things a teen girl does; she got her driver’s license and is active in sports. It’s the best result we could have hoped for,” says Zafar.
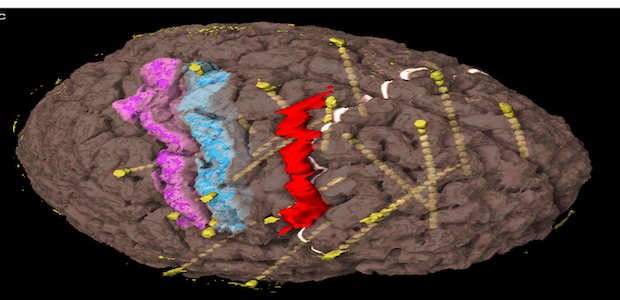
Image of the patient's brain with the red area showing the area of resection. Blue and red areas are motor and sensory areas of the brain.
