Duke One of Few Centers in Country to Offer CAR T-cell Therapies
Earlier this year, Duke joined a select group of medical centers across the country certified to offer both of the chimeric antigen receptor (CAR) T-cell therapies approved by the US Food and Drug Administration (FDA). It is now the only center in the region—South Carolina, North Carolina, and Virginia—offering either therapy.
The first FDA-approved CAR T-cell therapy, tisagenlecleucel (KYMRIAH), was approved in August 2017 for the treatment of patients up to 25 years of age with acute lymphoblastic lymphoma (ALL) that has relapsed or is refractory to therapy. The second, axicabtagene ciloleucel (axi-cel, YESCARTA), was approved in October 2017 for use in adult patients with large B-cell lymphomas whose cancer has progressed after receiving at least 2 prior treatments.
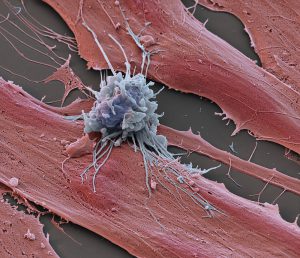
As the first FDA-approved gene therapy product, CAR T-cell therapy is unlike any other cancer treatment, relying on the patient’s own T cells to destroy cancerous B cells. In clinical trials, treatment with tisagenlecleucel resulted in an 81% overall 3-month remission rate in patients with ALL, a disease with few treatment options that historically has had poor outcomes. Remission was found to be durable, with no requirement for additional therapy in up to 50% of cases. Clinical trials with axi-cel demonstrated that the therapy was able to double patients’ long-term survival rates.
CAR T-cell therapy is an exciting step in the ongoing transformation of the cancer treatment landscape, says Paul Martin, MD, PhD, chief of Duke’s Division of Pediatric Blood and Marrow Transplantation.
“There is a lot of momentum toward developing immunotherapies for cancer treatment,” he says. “CAR T cells can be designed to attack almost anything on the surface of cancer cells, so as technology gets better, we should be able to manufacture CAR T cells that are specific to smaller and smaller groups of patients. In 30 to 40 years, people are going to think we were crazy for only using surgery, radiation therapy, and chemotherapy to cure cancer.”
Approval to offer the therapy requires a site to be certified as an authorized treatment center and for the site’s medical professionals to complete FDA-mandated training. Duke’s selection and approval as an authorized treatment center was enabled by its pre-existing infrastructure and expertise for treating high volumes of patients with hematologic malignancies as well as for managing the adverse effects associated with CAR T-cell therapy.
“Duke has a long history of developing cancer vaccines, being on the cutting edge of allogenic transplant immunotherapy, and, now, being involved in multiple engineered T-cell immune-based therapies,” says David Rizzieri, MD, associate director of Clinical Research in Duke’s Hematologic Malignancies & Cellular Therapy Program. “This allows us to have an in-depth and broad discussion with patients concerning both any reasonable treatment options currently available as well as clinical trial options that may be appropriate for them to consider.”
Martin and Rizzieri caution that CAR T-cell therapy is not without its risks. Adverse effects can include high fever, serious flu-like symptoms, sudden drops in blood pressure, and seizures. Reimbursement for the treatment is also still a challenging issue that is being addressed at centers across the country. However, the new therapies are an exciting step forward in providing a potentially curative option for patients with cancer that has failed other forms of treatment.