The clinical influence of an equation used by physicians since 2009 to incorporate an African American modifier into the estimated glomerular filtration rate (eGFR) may be replaced in the future by Duke laboratories.
Citing racial bias in the use of an algorithm that adjusts the creatinine clearance measure based on a patient’s race as identified by the EHR, a Duke Health task force recommended in a report to senior medical leadership in January that two adjustments be made to future eGFR measures:
- Require all blood chemistry tests that record creatine with eGFR value report one eGFR value using the Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) without the African American coefficient for every patient.
- Include a comment section in every eGFR result on every patient’s chart that reports both the value of the non-modified eGFR and the modified eGFR with the African American adjustment.
The Duke Health task force was formed as a response to an October 2020 petition signed by more than 250 Duke medical students, fellows, and medical staff, and presented to senior physician leaders asking the institution to eliminate or change use of the eGFR race coefficient. During the past two years, medical institutions across the U.S. have been reconsidering the use of modified eGFR data because of concerns about racial bias.
When the African American equation is applied, the test results artificially inflate the rate of filtration and is an indication of better kidney function, potentially delaying care for African American patients and/or preventing early assessment for transplant as kidney disease progresses.
Responding to both the student petition and task force, Duke’s medical leadership has agreed to consider the requested changes but wait for guidelines from the American Society of Nephrology (ASN). In April, an interim report from a National Kidney Foundation and ASN task force agreed that race modifiers in equations to estimate kidney function are problematic and that current race-based questions should be replaced.
Variations in Metrics Ascribed to Race
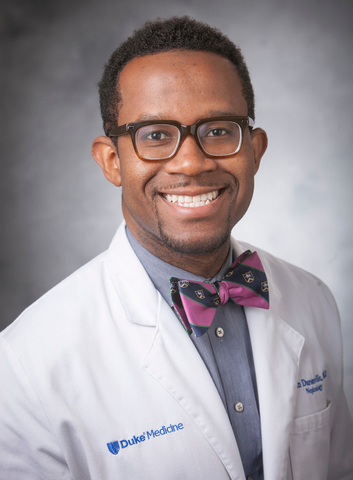
John V. Duronville, MD, a Duke nephrologist who co-chaired the task force and helped the students prepare their petition, says nephrologists have recognized the deficits presented by the adjusted eGFR for many years.
“These variations can only be ascribed to race, but we know from the human genome studies that race markers do not exist,” Duronville says. “There is no genetic difference identified to support a race coefficient in eGFR. Race by itself is a sociohistorical political construct, not biological.
The CKD-EPI measure, created in 2009, was preceded by the MDRD (Modification of Diet in Renal Disease) equation developed in 1999 to measure eGFR. It was developed following testing to achieve an objective measure of the dietary effects of protein in patients with kidney disease.
Accepting Modified eGFR at Face Value
“As a medical community, we have taken these measures at face value for years,” Duronville says. “But we are watching professionals inside and outside medicine pose questions about whether race has become a physiological determinant of any health outcome. We believe it’s time to reconsider this metric.”
Members of the Duke task force that made the recommendations included, in addition to Duronville, co-chair Michael Datto, MD, PhD, associate vice president for Duke University Health System Clinical Laboratories, vice-chair for clinical pathology and medical director for clinical laboratories; nephrologist Kimberly Evans, MD, Maestro Care; John Toffaletti, PhD, laboratory medicine; John Roberts MD, transplant nephrology, Jennifer Gommer, PharmD (transplant pharmacy), Racquel Holmes, MD, nephrology fellow; and medical students Nali Gillespie, Elena Drews and Norah Karlovich.