Established in 2009, Duke Health’s Adolescent Metabolic and Bariatric Surgery (MBS) program is one of the few centers earning both credentialing and certification from the American College of Surgeons Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program Standards (MBSAQIB) as a Center of Excellence.
“We were one of the first adolescent MBS programs in North Carolina and have completed rigorous quality and outcomes evaluations to earn accreditation,” says Sarah C. Armstrong, MD, pediatric medical weight management specialist and co-director of the Duke Center for Childhood Obesity.
Duke Children’s offers MBS for patients age 14 to age 23, which aligns with the latest American Academy of Pediatrics (AAP) practice guideline for the evaluation and treatment of children and adolescents with overweight and obesity. Armstrong is chair of the AAP Section on Obesity and significantly contributed to the updated guideline.
“It’s important for pediatric providers to consider bariatric surgery as one of the treatment options for teens with severe obesity, especially for those with additional health problems. We can discuss surgical options with families, and can offer medications or other lifestyle coaching support,” says Armstrong.
To refer a patient to Duke Children’s Healthy Lifestyles for adolescent MBS consideration or support with pediatric obesity, call 919-620-5394.
Comprehensive treatment options
“Obesity treatment requires a family commitment,” says Susan Thornton, RN BSN, MPH, clinical services nurse for the Duke Children’s Healthy Lifestyles and Metabolic Weight Loss Surgery program.
After a referral to Duke Children’s Healthy Lifestyles, patients and their caregivers consult with Thornton by discussing their goals, what they’ve previously tried, and barriers or challenges they’ve faced to decide the best patient-centered treatment option.
Some patients don’t qualify or want surgery and opt for alternative options like obesity medications, mental health counseling, nutritional counseling, or participation in the community outreach program Bull City Fit. Other patients meet the criteria for bariatric surgery and start that process.
Adolescent MBS criteria
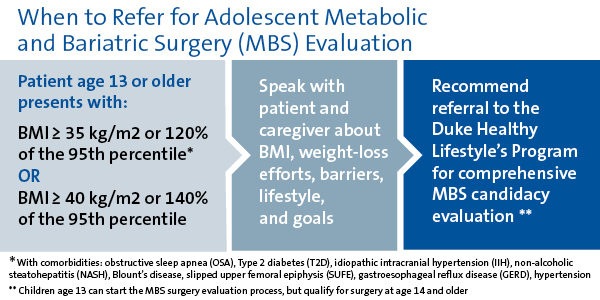
BMI and age are the key criteria for adolescent bariatric surgery. “Patients age 13 and older can start exploring surgery if they meet the AAP practice guideline criteria,” says Armstrong.
Adolescent MBS criteria:
- BMI ≥ 35 kg/m2 or 120% of the 95th percentile with clinically significant comorbid condition
- BMI ≥ 40 kg/m2 or 140% of the 95th percentile
Comorbidities include obstructive sleep apnea, Type 2 diabetes, idiopathic intracranial hypertension, non-alcoholic steatohepatitis, Blount’s disease, slipped upper femoral epiphysis, gastroesophageal reflux disease, and hypertension.
While insurance coverage for surgery begins at age 14, completing pre-surgery evaluations takes at least six months so patients can start the process at age 13.
The pre-surgical approval process involves a series of physical and mental health assessments, as well as consultations with dieticians and physician therapists to modify diet and physical activity.
Throughout this process, the team may identify contraindications, which include:
- a medically correctable cause of obesity
- current or recent history of substance misuse
- current or planned pregnancy within 12–18 months
- inability to adhere to post-operative dietary and medication regimens, including any medical, psychiatric, psychosocial, or cognitive reason for noncompliance
“Surgery may not be the best option after all,” says Armstrong. “The most important thing is to start the dialogue with patients so they can make informed choices.”
Surgical and long-term outcomes
Duke Children’s adolescent MBS procedures are often performed by weight-loss surgeon Dana D. Portenier, MD, using minimally-invasive techniques similar to adult procedures, including gastric sleeve with laparoscopy. Gastric sleeve has a shorter recovery time and preserves the opportunity for future procedures like gastric bypass later in life.
Post-surgery, patients follow up with surgical and Duke Children’s Healthy Lifestyles teams to monitor healing and progress. “Patients will need to check labs and maintain their healthy lifestyle after surgery to achieve positive surgical outcomes long term,” says Armstrong.
