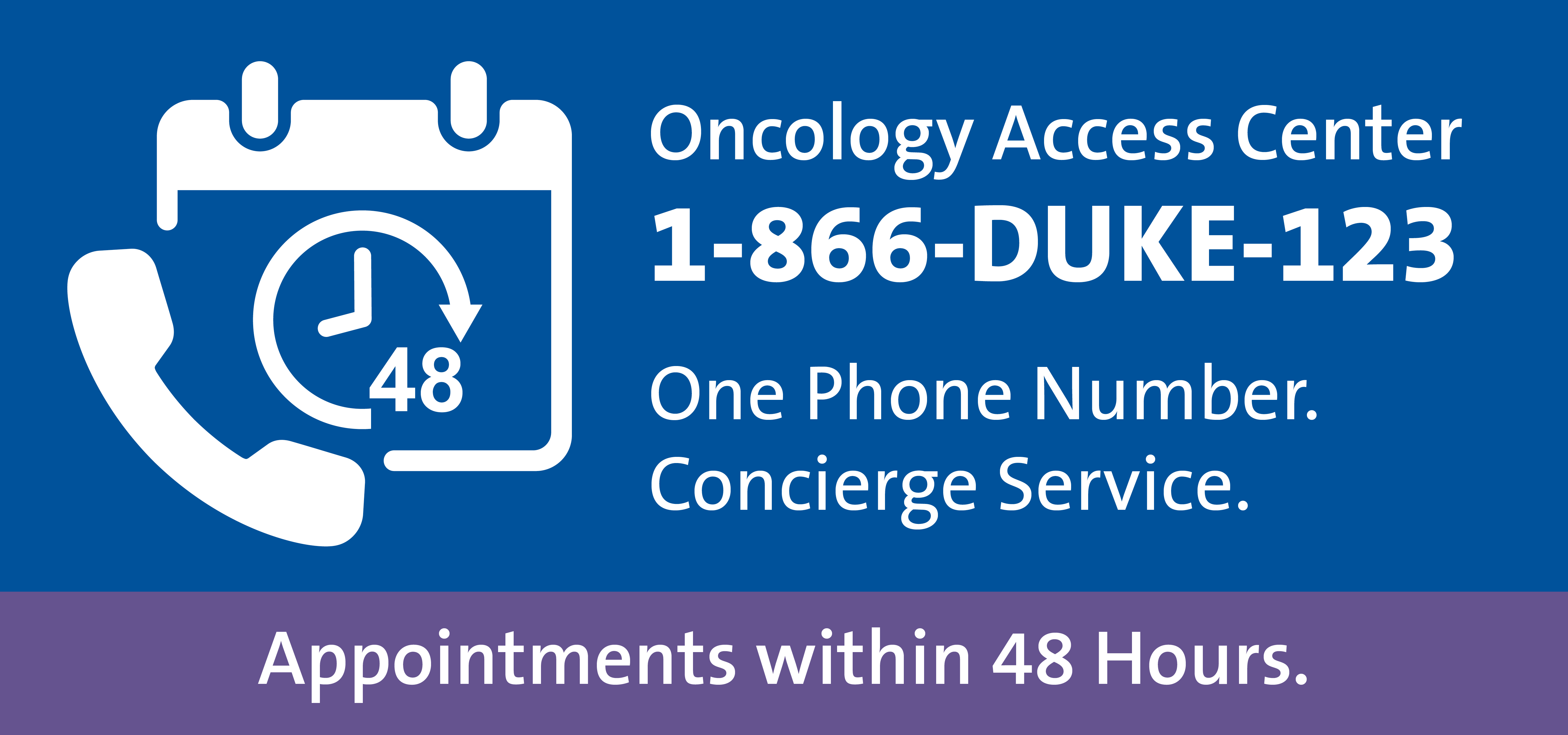
For patient referrals, call the referring provider team Monday through Friday between 8:00 a.m. and 4:30 p.m. at 866-385-3123 (1-866-DUKE-123) or email OncologyReferral@Duke.edu.
Duke Genitourinary Medical Oncologist Andrew J. Armstrong, MD, MSc, leads many of Duke Cancer Institute’s prostate cancer trials. The team has about 20 trials running, with seven actively enrolling. Several are open in Wake County and Durham, which increases access for more patients in North Carolina communities.
“We are on a mission to find novel strategies to prolong the survival of our patients or delay disease progression while preserving good quality of life,” says Armstrong.
Trials open in Wake County and Durham
ARCTIC
ARCTIC is a correlative multi-center study that examines circulating tumor cell biomarkers that may help predict hormone-resistant prostate cancer, and to what treatment patients will better respond. “Through a blood draw, we isolate circulating tumor cells and examine their mRNA expression. We want to know what makes those cells active and resistant to hormone therapy. This may lead to better precision therapies for patients,” says Armstrong.
CHAMP
This phase two trial, currently open for enrollment, tests if a combination of chemotherapies and immunotherapies (carboplatin, cabazitaxel, nivolumab, and ipilimumab) slows cancer growth in patients with metastatic neuroendocrine or aggressive-variant prostate cancer. Armstrong explains that the goal is to prolong survival and halt disease progression while maintaining acceptable toxicity.
SYNERGY-201
This new multi-center study is built upon Armstrong’s previous research findings, demonstrating that combining C-X-C motif chemokine receptor 2 (CXCR2) inhibition and androgen receptor (AR) targeting may prevent the transformation of typical prostate cancer into a more aggressive form, delaying hormonal resistance while also activating the immune system to improve outcomes in men with hormone-resistant prostate cancer.
The phase two study tests the combination of SX-682 and enzalutamide in men with mCRPC who have failed abiraterone therapy. “We want to intervene before a neuroendocrine transition takes place, restoring sensitivity to hormonal therapy to keep patients in remission longer,” says Armstrong.
EVOPAR-PR01
Duke will soon be a site for this phase three global study testing standard-of-care hormonal therapy in addition to the PARP1 selective inhibitor saruparib (AZD5305) for patients with newly diagnosed metastatic castration-sensitive prostate cancer (mCSPC). Previous studies show that PARP1 inhibitors in combination with hormonal therapies improve overall and progression-free survival in men with metastatic hormone-resistant prostate cancer, but moving this earlier before hormone resistance is an important next step. Urologic Oncologist Jeffrey W. Shevach, MD, is a PI in this study and practices in Wake County. “We are uniquely intervening earlier in the disease process with novel therapies to try to prolong survival,” says Armstrong.
Trials open in Durham only
PRESERVE-006
“We hope to find that combining the ‘smart bomb’ of radioactive therapy with immune therapy prolongs remission. It’s the first study of its kind for prostate cancer,” says Armstrong. This phase two multi-center study is for patients with mCRPC who’ve had PSMA-positive scans and disease progression on androgen-resistant pathway inhibition. It will examine the safety and efficacy of an immunotherapy called ONC-392 in combination with lutetium Lu 177 vipivotide tetraxetan (PSMA targeting standard of care radiation therapy).
COMBAT
The COMBAT study will launch soon for patients without PSMA expression or who have progressed after PSMA radioligand therapy. The study will test the safety and efficacy of 67Cu-SAR-BBN in patients with Gastrin Releasing Peptide Receptor (GRPR)-expressing metastatic castrate-resistant prostate cancer who are ineligible for lutetium Lu 177 vipivotide tetraxetan.
“About 15% of patients don’t have PSMA, so many could benefit from this potential therapy,” says Armstrong. “We’re testing if 64Cu-SAR-BBN, a copper agent used via a PET scan, can more accurately detect cancer, and if 67Cu-SAR-BBN radioactive therapy can target GRPR and attack cancer.”
