Dietary fatty acids can improve long-term health, according to a Duke endocrinologist and international lipidology expert, and they offer beneficial effects for a variety of conditions ranging from arthritic inflammation to cognitive impairment to depression.
Duke Lipid Clinic Director John R. Guyton, MD, is an ardent advocate for the use of omega-3 acid ethyl esters and fish oils, with one caveat. “The supplement is generally well tolerated, and I recommend it carte blanche and fully in women,” Guyton says. “Even in men, if I see situations in which it could be helpful, I suggest its use with a disclosure about a possible prostate cancer concern, though there is not yet a direct link in the research.”
A few patients resist fish oil supplements because of reflux or diarrhea symptoms, Guyton says, while others do not like the taste. But randomized controlled trials have demonstrated that fish oil is effective in lowering triglyceride levels and offers potential benefits such as reducing arthritic inflammation, giving a small memory boost for patients experiencing mild cognitive impairment, and contributing to the reduction of arterial inflammation, which may benefit cardiovascular health. The use of fish oil may also offer some benefit to patients with symptoms of depression.
His omega-3 advocacy is just one dimension of Guyton’s promotion of a nutritional approach that incorporates healthy lipids while avoiding others, notably his guidance to replace saturated with polyunsaturated fats to lower risk of coronary heart disease.
Guyton was among the physician leaders who founded the Southeast Lipid Association, the National Lipid Association, and the American Board of Clinical Lipidology. He has served as president of each organization and is currently Editor-in-chief of the Journal of Clinical Lipidology.
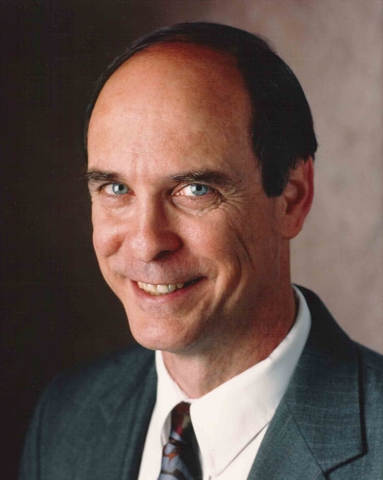
AHA advisory offers definitive guidance
Guyton cites the American Heart Association Presidential Advisory published in Circulation in 2017 as definitive guidance for clinicians offering nutritional advice for patients at risk of cardiovascular disease. Well-performed randomized clinical trials in the 1960s and 1970s showed that replacing saturated fats with polyunsaturated oils led to an approximately 30 percent reduction of heart attacks and strokes. “Importantly,” Guyton recalls, “those were not low-fat diets. However, manufacturers began to hydrogenate the good polyunsaturated oils, producing terrible trans fats, examples being stick margarine (but not tub margarine) and semi-solid white shortening. As the cardiovascular hazards of trans fats emerged, recommendations shifted to a low-fat message.
“But the low-fat reaction against trans fats led into another problem,” Guyton says. “While the obesity epidemic cannot be blamed entirely on the low-fat message, diets that are low in fat and high in carbohydrates tend to promote obesity. Then it came full circle, because obese humans produce their own saturated fat from carbohydrates.”
Despite growing public interest in dietary supplements such as omega-3s, Guyton cautions that the most recent dietary trends—particularly those encouraging more butter and other saturated fat in the diet—work against the lessons learned fifty years ago. A new fad, coconut oil, is especially problematic.
“Coconut oil in research has helped to induce coronary heart disease in rats and dogs. It is one of the worst saturated fats and there is no data suggesting its use,” he says.