A Duke vitreoretinal surgeon was among the authors of a recent JAMA Ophthalmology special communication urging rapid development of a revised classification system that could contribute to more robust measurement tools for acute-phase retinopathy of prematurity (ROP).
Cynthia Toth, MD, a Duke imaging researcher and surgeon, joined ophthalmologic colleagues from the ROP workgroup of the International Neonatal Consortium (INC) to advocate for a dynamic scale that would allow clinicians to record more precise data for clinical trial research.
The authors suggest in the December 13 special communication that future clinical trial data will be significantly enhanced by the greater precision offered from an improved ROP activity scale.
“The key issue for this group of authors is that the current ICROP (International Classification of ROP) classification does not help distinguish small changes in disease that clinicians know are present,” says Toth. “During examination, clinicians may observe multiple additional retinal findings, but there is no routine and categorical method to annotate or communicate these findings outside of the longstanding ICROP.”
The ICROP was developed before the onset of the use of anti-vascular endothelial growth factor therapy (VEGF) in the treatment of some cases of ROP, according to the special report. The use of such treatments alters the pattern of disease regression and recurrence.
ROP in its most severe forms can result in retinal detachments and in some infants can result in a lifetime of blindness, Toth says. Clinical trials have resulted in treatments that prevent vision loss in many of these infants. “As a retinal surgeon, I care for infants with the most challenging disease, for whom current treatments may not work,” she adds. “We need to encourage measurements that will lead to more effective research to support the development of new therapies.”
The INC’s ROP workgroup includes global leaders from across the field of pediatric ophthalmology, Toth says. The group’s work has focused on improving the infrastructure and tools needed to improve clinical research for pediatric patients with ROP. “This group has helped identify some of the variables and disease markers that may be useful in the future,” she says. “This includes findings from novel imaging in these infants using optical coherence tomography (OCT) imaging.
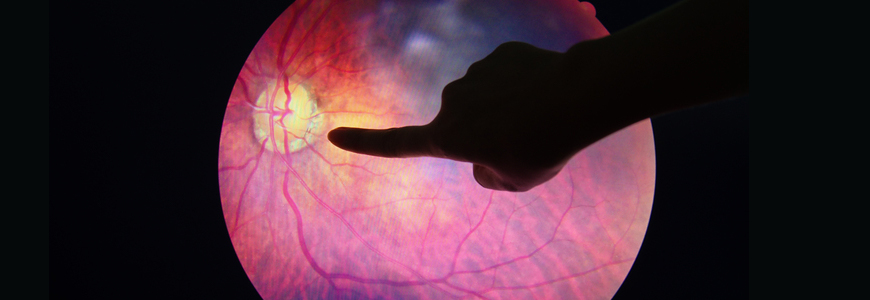
Sharon Freedman, MD chief of pediatric ophthalmology at Duke, expressed optimism about the future of OCT. “While standard clinical examination of premature infants has been accomplished for years by experts using indirect ophthalmoscopy to visually detect and monitor ROP, OCT offers an exciting non-invasive modality,” Freedman says. “Dr. Toth and her colleagues at Duke pioneered the application of this amazing imaging technique to premature infants at the bedside, allowing detection and monitoring of retinal changes at levels of details previously unimaginable.”
Freedman adds: “Comparing standard clinical examination findings to those detailed changes now make it possible to identify and document with OCT, which opens the way to improved understanding of the pathophysiology and treatment for ROP.”
Toth is careful to note that the authors of the special communication do not attempt to prove the existence of additional, more dynamic markers, but they advocate for research that may help quantify them. “We are saying that these markers may be very, very important if we are going to follow patients to monitor deviations from development or changes in disease processes after treatment,” she says.