When a 65-year-old woman from Florida with a 10-year history of spine problems presented to Duke Orthopaedics, her spine was curved forward so severely from scoliosis and kyphosis that she was facing the ground instead of straight ahead, tilting to the right and unable to stand up or lift her head. 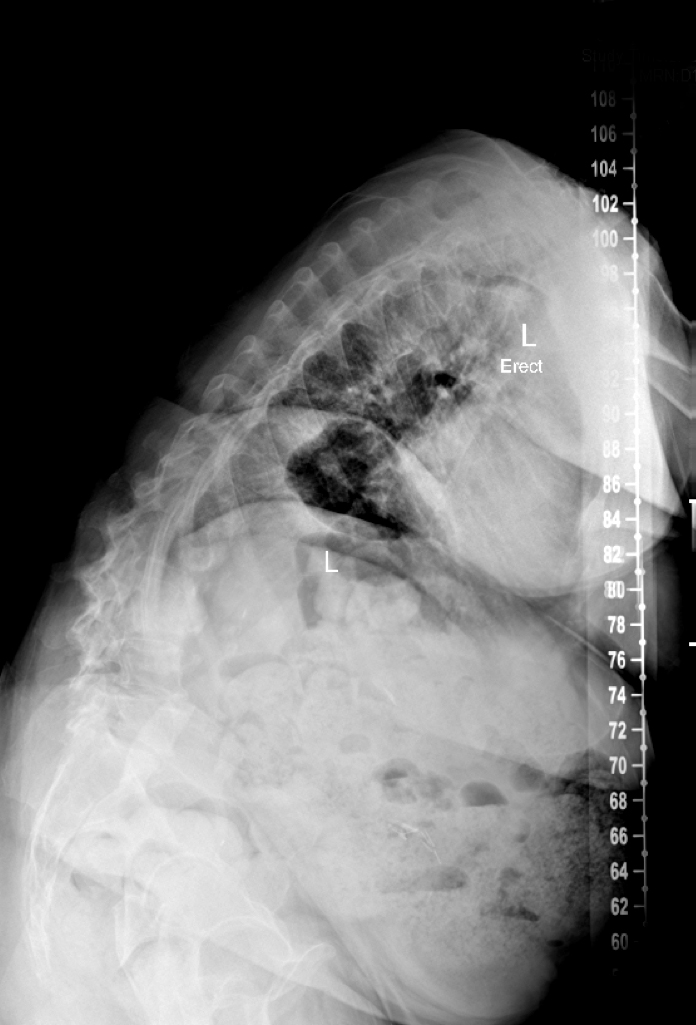
She had consulted with several local physicians and had tried many therapies to alleviate her constant debilitating pain, including physical therapy, injections, and narcotic medications at dosages so high that they could be lethal in some people. None of these treatments helped, and her pain was worsening.
Because of the severity and complexity of her scoliosis, the patient was referred to Isaac Karikari, MD, a neurosurgeon and spine surgeon who specializes in treating complex spinal deformities. “She was in a terrible state when I first saw her, and her condition wasn’t compatible with any reasonable quality of life or ability to function normally.”
The patient used a walker and stood with positive sagittal malalignment and a truncal shift to the right. She was severely bent over and any attempts by her to straighten her body resulted in incapacitating pain. “Complex spinal fusion surgery was the only option,” says Karikari.
The patient underwent two months of physical therapy to prepare her body for surgery. “Before we recommend such extensive surgery we make sure that the patient’s quality of life is being significantly impacted by the condition and that they are in the best physical shape possible, because this surgery is not trivial; in fact, it is amongst the most complex spinal procedure performed nationwide,” Karikari explains.
Question: What procedure did Karikari perform to straighten the patient’s spine, reduce her pain, and improve her quality of life?
Answer: Karikari performed pedicle subtraction osteotomy involving the area from the C4 cervical vertebra to the pelvis.
“Basically, we cut her spine in half by removing a wedge of bone and artificially creating a curvature in her lower spine then put it back together again,” says Karikari. The surgery is performed with a complex team of anesthesiologists, nurses, neuromonitoring experts, and employs the most advanced technology. “We take advantage of new technology at Duke to make surgeries like this safe and successful,” he says.
The procedure involved first exposing the spine from the fourth thoracic level to the sacrum. Following exposure, screws were inserted into the bone to serve as anchors. “We’re able to perform this very safely now with intraoperative CT scan,” says Karikari.
After the screws were placed, the team proceeded with the most challenging part of the surgery: disarticulating the spine by cutting a wedge out of the bone. “We have to work around delicate nerves and make all efforts to protect the nerves. The surgery took about 10 hours to execute. Our dedicated anesthesia team, excellent nursing team, and other operating room personnel are a vital part of the procedure and honestly are the ones that make this surgery such a success at Duke,” says Karikari.
After a week-long hospital stay, the patient underwent rigorous rehabilitation. Six months postoperatively she was standing fully upright and her pain had subsided. 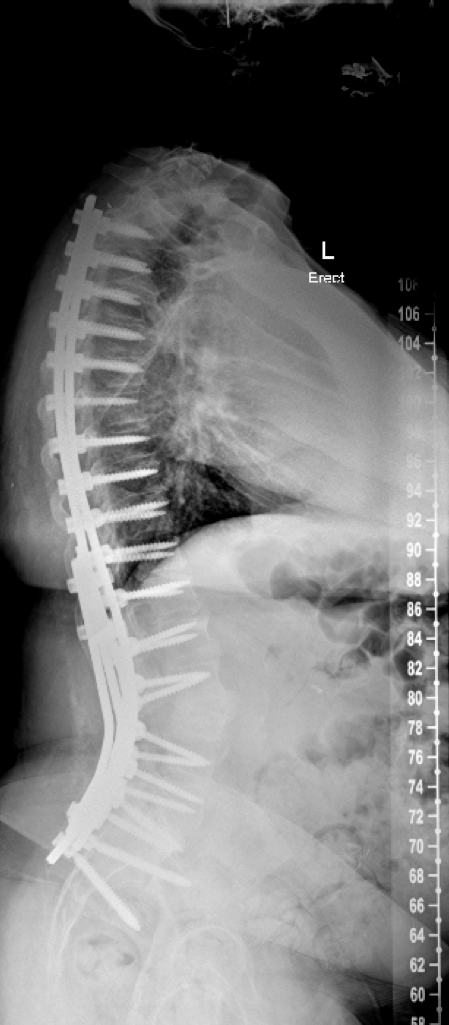
During a follow-up visit with Karikari the woman told him she was again able to enjoy one of her favorite activities: “She has a window over her kitchen sink that looks out onto the street, and she watches children playing and people passing by while she’s washing dishes,” says Karikari. “She couldn’t do that for a long time because of her condition, but she’s now able to look out that window again and she loves it.”
