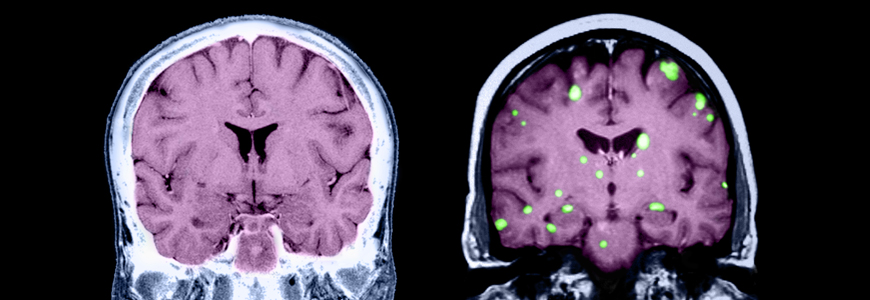
As the population of cancer survivors increases in the United States, the overall incidence of cancer metastasizing to the brain and spine is increasing as well, with an annual estimate of more than 280,000 new cases from all cancer types. In response to this growing need for patient care, several personalized medicine trials are now available through the Duke Center for Brain and Spine Metastasis (DCBSM), one of the only research programs of its kind.
The center—led by neurosurgeon Peter E. Fecci, MD, PhD, medical oncologist Carey K. Anders, MD, spine surgeon C. Rory Goodwin, MD, PhD, and radiation oncologist John P. Kirkpatrick, MD, PhD—was established in 2017. Anders, the DCBSM medical director, notes that there has been a true paradigm shift over the past few years of historically excluding patients with brain and spine metastases from clinical trials to designing trials specifically for them prior to local therapy.
“These patients—especially those with leptomeningeal disease—have historically been excluded from participating in any type of clinical trial opportunity due to a history of central nervous system disease,” she says. “At Duke, our focus is on developing trials that are geared toward these patient populations, the specific types of molecular alterations that the metastasis may have, the side effects of treatments, and quality-of-life considerations that are very unique to this patient population.”
Designing Personalized Medicine Trials
The DCBSM’s trials span multiple disease groups and study multiple aspects of brain and spine metastasis, says Amanda Van Swearingen, PhD, a DCBSM senior research associate. Due to the COVID-19 pandemic, several clinical trials are still in the process of being opened, but four major studies have been opened through the DCBSM to enroll participants:
Alliance A071701: This genomically guided treatment trial is designed for patients with brain metastasis across any primary solid tumor type that has any of several specific molecular alterations. It highlights the multidisciplinary nature of the DCBSM’s offerings, Anders notes, as the treatment involves resection, radiation, and molecularly targeted therapy.
A lot of personalized medicine uses specific drugs that can't penetrate the blood-brain barrier at all or sufficiently enough to be therapeutically effective,” Van Swearingen adds. However, newer medications like the ones used in this trial are known to have greater brain penetrance and may be better suited to targeting the driver mutation in patients with brain and spine metastasis, she says.
BMX-MBM-001: This trial is designed for patients who will receive whole-brain radiation therapy because they have 10 or more brain metastases. Patients will either receive BMX-001—a drug developed at Duke—prior to radiation or radiation only. The study will analyze whether the drug can prevent or minimize neurocognitive side effects during treatment to improve patients’ quality of life, Van Swearingen says.
Neoadjuvant Immunotherapy in Brain Metastases: This randomized trial is designed for patients with brain metastasis from multiple primary solid tumor types. Patients who are planned for a standard-of-care resection of their brain metastases will be enrolled. In the presurgical treatment phase, patients will receive a single dose of two immune checkpoint inhibitors or no immunotherapy prior to surgical removal of their brain metastasis followed by stereotactic radiosurgery (SRS). All patients will receive immunotherapy after surgery and SRS. “Starting treatment with these agents prior to surgery, as opposed to afterwards as they are typically given, may improve the response to therapy without delaying surgery,” Van Swearingen explains.
MRI for Assessing Spinal Metastases: This trial is designed for patients with spine metastasis from any cancer to determine if quantitative MRI can objectively measure changes in the spine and metastasis to it after stereotactic body radiation therapy (SBRT). Quantitative MRI may enable physicians to identify if any damage to the vertebral body or spinal cord occurred with the high-dose radiation delivered by SBRT, as well as measure and perhaps predict outcomes, including response to treatments. Van Swearingen highlights that being able to accurately monitor and predict how the spine and any metastases are responding to interventions may help with alleviating the pain that often accompanies spine metastasis.
The research portfolio also includes non-interventional registry studies to observe outcomes for patients with brain and spine metastasis, as well as first-in-human Phase 1 trials with novel targeted inhibitors, that will inform future studies.
Fast-tracking Regulatory Protocols
Future clinical trials from the DCBSM will focus on systemic therapies that can pass through the blood-brain barrier to more adequately reach tumors and will analyze intracranial tumor response to immune-based therapies. Van Swearingen emphasizes Duke’s commitment to working toward expediting the approval of trial protocols whenever possible, particularly for patients with leptomeningeal disease whose survival may be only a few weeks to months.
“For this patient population, literally every week is of the essence, and being able to say that we can open a study efficiently and as quickly as possible is really critical,” she says. “We also want to be able to go from the bench to the bedside and back. We are committed to fostering preclinical and basic science that will lead not only to novel therapeutic approaches but also enable rapid translation of these strategies to the clinic. To that end, we are building this capacity through collaborations and infrastructure within the DCBSM.”