Cardiology and Oncology Combine Forces
A collaborative specialty at the intersection of cardiology and oncology helps patients diagnosed with cancer mitigate the potential side effects of cancer or cancer treatment on the heart and cardiovascular system.
Patients with cancer are increasingly referred to the Duke Health cardio-oncology team for assessment and management of cardiovascular disease (CVD) and its complications.
“This is an emerging specialty that is becoming better at understanding the role of heart disease and heart-related complications in patients being treated for cancer,” says Michel G. Khouri, MD, 1 of 3 cardiologists who have expanded the clinic through grassroots outreach to oncologists.
By protecting the heart prior to the initiation of chemotherapy, Khouri says, patients can avoid heart-related complications that have the potential to interrupt cancer treatment. Khouri and his colleagues encourage oncologists to request a cardiovascular assessment prior to initiating treatment for patients with existing CVD and for patients starting treatments that have potential heart-related side effects.
Traditionally, patients have been referred to cardiologists when heart-function issues were observed during treatment. “Sometimes we have to stop cancer treatments because of heart muscle injury,” Khouri says. “Our objective is to mitigate the risks of injury proactively. We want to move beyond waiting for cardiac symptoms before taking action. If we can protect the heart earlier,” he explains, “we can help ensure the best long-term cancer and heart outcomes.”
Widely used chemotherapy drugs—notably anthracyclines and trastuzumab—can cause cardiotoxicity. Some patients have signs of cardiotoxicity before developing any symptoms of sickness. Other risk factors, such as diabetes mellitus, hypertension, and unidentified underlying CVD, can add risk and complexity to drug therapy.
Various cardiovascular medications used in patients with hypertension, high cholesterol, and heart failure have demonstrated the capacity to act as cardioprotectants during chemotherapy. Cardio-oncologists may use them in patients with higher cardiac risk or to help promote heart recovery in patients who have already developed cardiovascular complications.
In addition to medications, the role of exercise training is an active area of research to determine if conditioning might be cardioprotective and help to mitigate the loss of stamina experienced by patients with cancer and those receiving cancer therapies.
Despite the availability of well-developed techniques to detect cardiovascular injury, cardio-oncologists have more to learn about identifying patients at the highest risk who are more in need of cardiac health evaluations and ongoing monitoring.
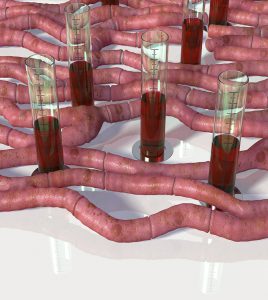
“Ongoing research with heart imaging techniques and blood tests will hopefully improve our ability to determine risk in the future,” Khouri says.
The clinic is just seeing “the tip of the iceberg,” explains Khouri. “We’ve helped many patients who would have been subjected to greater cardiac risk and helped others recover heart function so they could continue their cancer treatment. Still, we need more proactivity in referring patients earlier.”