To refer a patient, call 919-684-3181 or email CancerGenetics@Duke.edu.
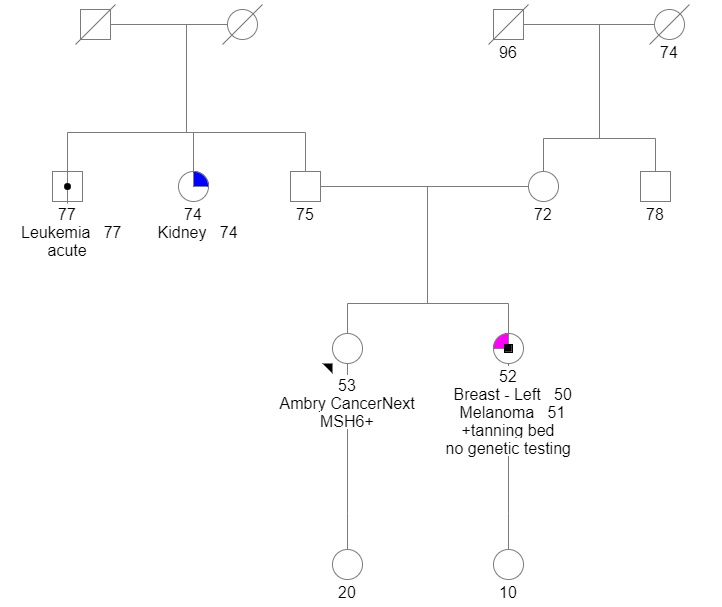
A 53-year-old female patient unaffected with cancer was referred to Brianna Cadalzo, MS, CGC, by the Duke Breast Risk Assessment Clinic. The patient met National Comprehensive Cancer Network (NCCN) criteria for high-risk breast cancer gene testing based on having a first-degree relative diagnosed with breast cancer at age 50 or younger.
After consultation with Cadalzo, the patient underwent a comprehensive 34-gene panel, which identifies inherited risks for at least eight types of cancer. Results revealed a pathogenic mutation unrelated to breast cancer: an MSH6 mutation consistent with a diagnosis of Lynch syndrome.
“If we only tested for breast cancer gene mutations, we would have missed these results. The patient was motivated to understand how her results influenced her cancer risk and health moving forward,” says Cadalzo.
What was the impact of these results and clinical recommendations?
“The mutation causing Lynch syndrome increases the risk for several cancers, including colon, uterine, and ovarian. While this patient reported no known family history of these cancers, the mutation alone significantly increases her cancer risk,” says Cadalzo.
After reviewing her results with Cadalzo, the patient was referred to Duke Health’s gastrointestinal and gynecology oncology teams to discuss a cancer surveillance plan and options to reduce cancer risk.
“This patient’s gynecologic oncology team recommended a hysterectomy with a bilateral salpingo-oophorectomy as a risk-reducing intervention,” says Cadalzo. “The patient agreed to move forward with that surgery.”
In addition, the patient scheduled an appointment with a gastroenterologist specializing in Lynch syndrome to assess gastrointestinal cancer risk and a personalized screening protocol. “Due to her higher risk for gastrointestinal cancers, the gastroenterologist will likely advise her to have more frequent colonoscopies and initiate regular upper endoscopies,” says Cadalzo.
In addition to genetic testing results, genetic counselors can also make recommendations based on family history alone. Cadalzo ran a breast cancer risk model for the patient, which revealed an estimated lifetime breast cancer risk of >20%. Thus, Cadalzo recommended that the patient discuss high-risk breast screening with her breast team. High-risk breast screening typically entails alternating between breast mammogram and MRI every six months.
The patient's genetic testing provided an unexpected finding that might have had negative health consequences if left undiagnosed. “The patient took a proactive approach to lower her lifetime cancer risk or at least catch it earlier if it develops. Testing may have also helped other family members, who now have awareness of the MSH6 mutation and may also choose to get tested for it,” says Cadalzo.
Patient's Hereditary Genetics: