A nine-year-old boy from Washington, D.C., had experienced epileptic seizures all his life. His mother’s concerns grew as the frequency increased to some 20 seizures a day, with 10 to 15 so severe that the boy would lose consciousness.
The boy had visited several large health-care institutions only to be told that his seizures could not be cured. These experts worried that his abnormality was seated in or so close to the motor cortex that surgery entailed too much risk of paralysis without an adequate likelihood of a cure. Aside from the seizures, the boy functioned well and was active in sports and school.
Unwilling to give up, the mother and son traveled to Duke to meet with epileptologist and pediatric neurologist Muhammed Zafar, MD.
Question: What options did Zafar believe Duke could offer to treat the boy’s seizures that other centers could not?
Answer: Zafar believed that Duke’s extensive experience with similar cases and advanced technology could reveal a path to treatment. Using an innovative electric source imaging technique that combines noninvasive high-density EEG and advanced MRI to create a three-dimensional brain model, Duke neurologists localized the brain abnormality to the supplementary motor area rather than the main motor cortex. Aided by a three-dimensional “augmented reality” model, pediatric neurosurgeon Matthew Vestal, MD, MBA, MHS, resected the problematic area, which completely relieved the patient’s seizures.
“We have a great deal of experience in treating children with refractory problems,” Zafar says, noting that Duke is a Level 4 epilepsy center, the highest designation for complex epilepsy care. “And we have developed some unique techniques that can help us.”
The multi-step process of identifying the source of the patient’s seizures began with the boy checking into the hospital for an inpatient epilepsy monitoring stay. Electrical activity in his brain was recorded using both a standard scalp EEG with 20 to 30 electrodes and a special high-density EEG with 100 to 200 electrodes.
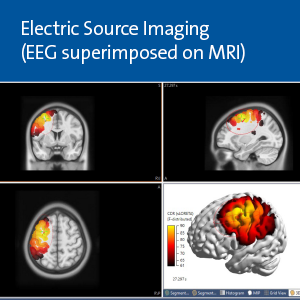
The next step was high-quality, advanced 3 Tesla MRI imaging of his brain. Zafar and his team have developed special algorithms to analyze these MRIs.
“Results of these two diagnostic modalities are combined and superimposed on each other in a process called electric source imaging. We can then precisely see in a three-dimensional model where the seizure signal is coming from, and use that three-dimensional brain model for localization and surgical planning,” Zafar says.
The imaging and analysis clearly indicated that the seizures did not originate in the main motor cortex, but rather in the supplementary motor area, which entails much less surgical risk. To confirm that finding, Vestal, a Duke pediatric neurosurgeon with a specialty in epilepsy, placed electrodes in the patient’s brain using a robotic stereotactic assistance system known as ROSA.
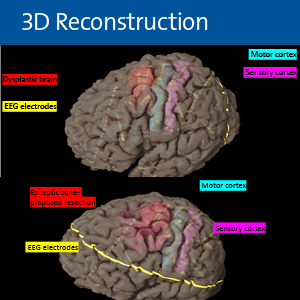
“When electrodes are sitting on the outside of your head, the electrical activity they measure has to go through a lot of material like the brain, skull, and skin,” Vestal says. “Placing electrodes in the brain involves a small surgery, but is actually minimally invasive and low risk. It involves using a robot and lots of pre-operative imaging to decide exactly where we could put the 12 electrodes. It allows us to localize precisely where the seizures are coming from down to the millimeter or submillimeter.”
The boy was monitored in the hospital again and allowed to have his seizures. “Our electrodes told us that our hypothesis was correct—all the pictures and all the electrical activity showed an abnormality in the supplemental motor area that dated from the time his brain was developing in the womb. We have had experience in doing similar things in similar children, so we thought we could give him a really good shot at being seizure-free forever,” Vestal says.
Vestal operated again to remove the electrodes and a section about the size of a golf ball from the supplementary motor area.
The surgeries were aided by special software unique to Duke that converts data into three-dimensional images. “When we get all of this data, rather than showing the surgeon an image on a two-dimensional screen, we put it into an ‘augmented reality’ app that shows a holographic view of the brain for planning the surgery,” Zafar says.
One predictable—and unsettling—side effect of this surgery is that the patient wakes up to temporary paralysis of the side of the body controlled by the affected portion of the supplementary motor area. But in the days and weeks that followed, the boy’s brain re-programmed to compensate, and he regained his movement and strength.
The surgery completely cured him of his seizures. “He is now back home in Washington, D.C., back in school, playing sports at grade level, and not having any seizures,” Vestal says.
To refer a child, sign into Duke MedLink or call 919-668-4000.