Bacterial Translocation from GI Tract May Contribute to Sepsis
New research highlights role of gut as cause of the multi-organ condition
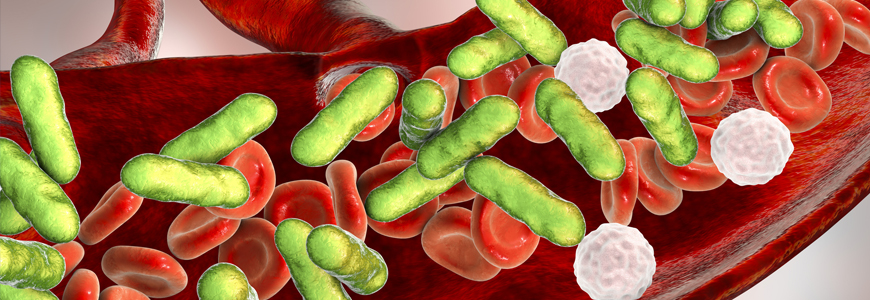
Bacterial translocation from the gastrointestinal (GI) tract may contribute to the multi-organ failure associated with sepsis, a Duke endocrine researcher reports in a recent study. Focused on metabolic changes associated with sepsis in tissues of the ileum, jejunum, skeletal muscle, liver, and lung, the study identified clues about the causes and progression of the condition.
Amro Ilaiwy, MD, a Duke endocrinology fellow, is the first author of The American Journal of Pathology study describing the metabolic relationships associated with sepsis. The goal of the study, Ilaiwy says, was to attempt to better understand the organ failure process associated with sepsis and to help develop more effective therapies that may be able to target the gut.
Much of the previous sepsis research, he says, focused on metabolic changes isolated in blood plasma. “The problem is that we were seeing many agents in the samples, but we were not sure of the sources of those agents,” he says. “This research represents a new approach that allowed us to review effects among different tissues to produce more informative results.”
At least 1.7 million American adults develop sepsis annually, according to the CDC, and nearly 270,000 of those adults die as a result. The condition is more common and more deadly in hospitals: the CDC reports that one in three patients who die during hospital stays have sepsis.
Based on animal research, the findings appear to indicate that the multiple significant changes observed in amino acids within plasma are likely originating within the GI tract. These metabolic changes are merely reflected in plasma analysis.
In the study, live Pseudomonas aeruginosa, isolated from a patient, was given via intravenous catheter to pigs to induce sepsis. Eighteen hours later, non-targeted metabolomic analysis using gas chromatography/mass spectrometry was used to analyze tissues affected by the bacteria. Pseudomonas aeruginosa has been identified as a common cause of sepsis in ICUs.
Among the key results:
- The ileum and liver demonstrated significant changes in metabolites involved in linoleic acid metabolism.
- The ileum and lung had significant changes in the metabolism of arginine/proline metabolism.
- The skeletal muscle and lung had significant changes in aminoacyl-tRNA biosynthesis, as analyzed by pathway analysis.
“As a clinician and a researcher, I also look at the bigger picture of what we can do with these findings,” Ilaiwy says. “The next step should be to look into therapeutic targets in the gut to try to identify an agent that could slow down these changes in the gut. If we can protect the gut during sepsis, we may achieve better outcomes.”