Aortic Models Take Shape With Medical Imaging, 3-D Printing
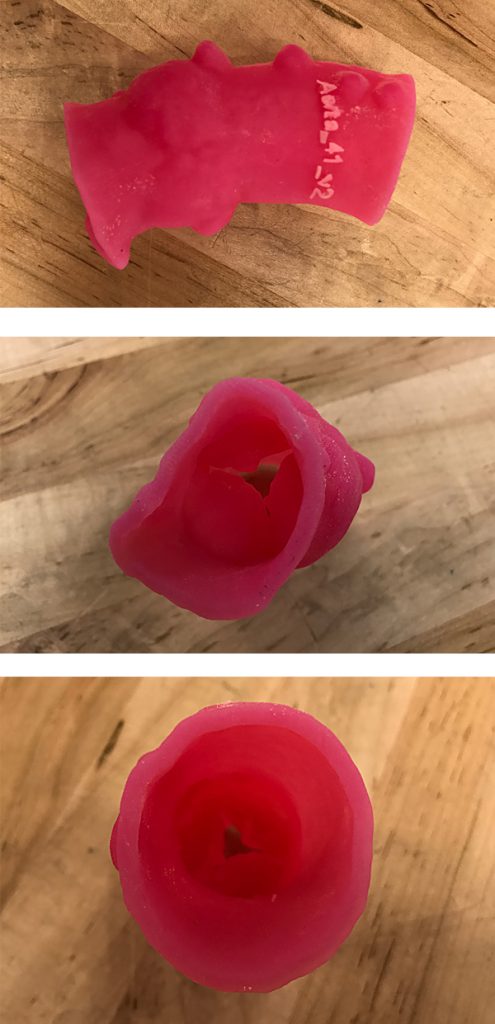
FIGURES: 3-D–printed models of the aortic valve assist in the the study of para valvular leaks and improve preparation for cardiac procedures. Creation of the replicas begins in the Multi-Dimensional Image Processing Lab at Duke Radiology. Technologists use images to create multi-dimensional, virtual models.
Using existing medical imaging and emerging 3-dimensional (3-D) printing technology, a Duke team creates anatomical models of the aorta and aortic root to study para valvular leaks and improve preparation for cardiac procedures.
The research effort is designed to generate more data about the effectiveness of anatomical models to prevent leaks in transcatheter aortic valve replacement (TAVR) and improve the effectiveness of mitral valve and left atrial appendage interventions. In conjunction with the research, Duke interventionists have used this technology to prepare for multiple successful procedures.
Anatomical models have been used for several years in TAVR leak assessments, says Sreekanth Vemulapalli, MD, the Duke cardiologist directing the research. But this effort is focused on assessing the effectiveness of models. The team is reviewing 20 blinded Duke cases of patients who underwent TAVR insertions before anatomical models were available. The team reviews post-insertion ultrasound imaging and the patient’s leak history to determine the device’s effectiveness.
“Leak assessments can be attempted with the use of CT scanning technology to simulate the insertion of the device in the aorta,” Vemulapalli says. “But it’s obviously more intuitive and powerful to physically replicate the procedure. 3-D printing appears to be the perfect response to this clinical problem.”
Creation of the replicas begins in the Multi-Dimensional (Multi-D) Image Processing Lab at Duke Radiology. Technologists use data from imaging modalities to create multi-dimensional virtual models of patients’ anatomical structures, which are then printed in a 3-D laboratory in conjunction with Duke engineering.
Strong clinical evidence supports the use of TAVR for both extreme-risk and high-risk patients with symptomatic severe aortic stenosis, and continued development of new valves makes implantation more reliable. In the majority of cases, imaging and pre-procedure assessment are sufficient to ensure minimal leakage. But Vemulapalli notes that more complex cases may benefit from modeling.
“The models give us a way to do a dry run and figure out whether leakage will occur,” he adds. “We hope to be able to leverage our research to take advantage of the many new devices to find a way to reduce leaks.”