Alternative to Standard Biopsy for Prostate Cancer Detection
A 58-year-old man was referred to Duke Medicine for evaluation of a history of elevated prostate-specific antigen (PSA). At a baseline screening in 2008, his PSA level was 1.8 ng/mL, but it had risen to 3.6 ng/mL by 2013. At the time of his referral, he had not received any empiric treatment for potential noncancerous causes of elevated PSA such as urinary tract infection, prostatitis, or benign prostatic hypertrophy (BPH). He had never had an ultrasound (US) examination of the prostate or a prostate biopsy. In January 2014, the patient saw Duke Medicine’s urologic surgeon Thomas Polascik, MD.
Dr. Polascik recommended magnetic resonance imaging (MRI) of the prostate as the next step to rule out cancer. Transrectal US (TRUS) is the most frequently utilized imaging procedure for detecting prostate cancer. However, multi-parametric MRI (mpMRI) can offer superior visualization of prostate anatomy and functional delineation of lesions. In this patient, the MRI revealed 3 abnormal areas in the prostate that were 2 cm x 8 cm, 1.3 cm x 0.9 cm, and 1 cm x 5 cm. At this point, a biopsy of the lesions was recommended.
Question: What alternatives exist to standard core biopsy in the evaluation of potentially cancerous lesions in the prostate?
Answer: The mpMRI-guided biopsy can be used in conjunction with TRUS-guided biopsy to target lesions more specifically.
|
|
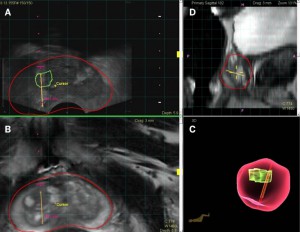
| Figure 1. mpMRI-TRUS guided biopsy. (A) target lesion located at the right anterior medial mid prostate; (B) MRI image of target lesion; (C) 3D model of the biopsy needle tract; (D) sagittal view of the prostate. In all images, red = contour of the prostate, green = contour of the targeted lesion, yellow = needle biopsy. | |

|
|
| Figure 2. (A) Target lesion hit as shown on TRUS and (B) MRI. In all images, red = contour of the prostate, green = contour of the targeted lesion, and yellow = needle biopsy. |
Duke Medicine is one of a handful of institutions in the country that performs mpMRI-guided biopsies to detect prostate cancer. The procedure is used in conjunction with TRUS and has been shown to be 2 to 3 times more sensitive than standard core biopsies, particularly in detecting high-grade or aggressive cancerous lesions of the prostate. Figures 1 and 2 to the right illustrate the targeting and biopsy of prostate lesions using mpMRI-TRUS technology.
“We recommended that this patient undergo an mpMRI-targeted biopsy, but there was a wait time of approximately 4 weeks, and he was anxious to get a diagnosis as soon as possible. So the patient opted for a standard TRUS-guided 12-core biopsy at that time,” Dr. Polascik explained.
The biopsy results showed no evidence of cancer. Given the findings of the initial mpMRI, however, Dr. Polascik then recommended that the patient still undergo the mpMRI-guided biopsy because it is more specific for targeting lesions than conventional biopsy.
This time, the biopsy did reveal cancerous loci in both sides of the prostate, and pathology indicated that the tumor was relatively aggressive, with a combined Gleason score of 7 (3 + 4).
“We talked about treatment options, and he underwent a robotic radical prostatectomy in April 2014,” Dr. Polascik said. The patient has since had an excellent recovery and outcome.
“His case presents a contrast,” Dr. Polascik commented. “He went through the conventional diagnostic pathway of the random 12-core biopsy, but it failed to detect his cancer, which was clinically significant and required treatment. We were able to offer him this more contemporary protocol using mpMRI technology to ascertain what kind of lesions were present in the prostate (and their size and location) and then, once we identified them, we could perform a targeted biopsy. It’s an improvement in both the MRI imaging modality and the targeting.”