Abnormal Retinal Vascularization
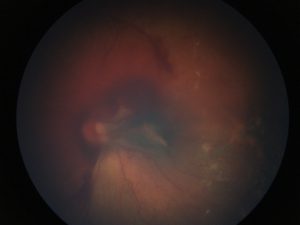 FIGURE 1. On initial examination while the patient was under anesthesia, vitreous and preretinal hemorrhage, vitreous contraction, and epiretinal membrane formation with macular traction were observed
FIGURE 1. On initial examination while the patient was under anesthesia, vitreous and preretinal hemorrhage, vitreous contraction, and epiretinal membrane formation with macular traction were observed
During screening for preterm infants, an infant born at 31 weeks of gestational age was observed to have abnormal retinal vascularization suggestive of retinopathy of prematurity (ROP). To slow and eliminate the growth of abnormal blood vessels, an ophthalmologist performed laser photocoagulation. However, the patient did not have adequate response, and the procedure had to be repeated 3 months later.
After the second round of treatment, the patient developed epiretinal scar tissue and bleeding in her left eye (Figure 1). She was referred to the Pediatric Retina and Optic Nerve Center at the Duke Eye Center to remove the scar tissue.
Question: What condition, often misdiagnosed as ROP, did the patient have, and how was it eventually diagnosed?
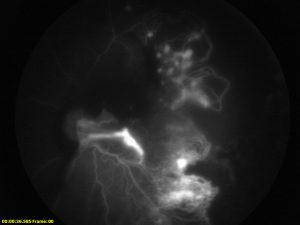 FIGURE 2. Fluorescein angiography illustrates marked macular and peripheral ischemia with dye leakage at the margin of the vascular and avascular retin
FIGURE 2. Fluorescein angiography illustrates marked macular and peripheral ischemia with dye leakage at the margin of the vascular and avascular retin
Fluorescein angiography, which was performed while the patient was under anesthesia, revealed that her peripheral retinas were poorly perfused. Coupled with findings on clinical examination, these results were consistent with a diagnosis of FEVR, a hereditary disorder that impairs vascularization of the peripheral retina.
Fluorescein angiography also demonstrated areas of persistent avascular retina (Figure 2). Vajzovic used the results of imaging to guide additional laser photocoagulation in both eyes and performed surgery to remove scar tissue. She also screened the patient’s family for the hereditary condition, so, if required, she could initiate their treatment as soon as possible as well.
Following laser therapy and surgery, Vajzovic reports that the patient’s eyes are doing well and will likely maintain good visual acuity (Figure 3).
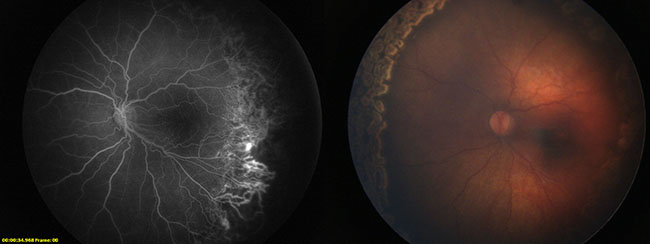
FIGURE 3. At the patient's 3-month follow-up visit after surgical intervention and additional laser photocoagulation treatment, both the hemorrhaging and macular traction resolved and a noticeable decrease was seen in dye leakage
When Lejla Vajzovic, MD, a pediatric retinal specialist, first examined the patient, she suspected that treating the patient’s condition would require more than the simple removal of scar tissue. “ROP made sense as her initial diagnosis, but when she had 2 rounds of treatment with the laser and her condition did not improve, we needed to start thinking outside the box.”
“It’s lucky that, because the patient was born preterm and underwent routine ROP screening, she was treated so early,” says Vajzovic. “Typically, when patients are born full term, they don’t get diagnosed until very late, which often means we are trying to catch up on treating their retinal detachment for the rest of their life.”
Still, Vajzovic cautions, early disease detection is not a cure. FEVR is a life-long disease, requiring yearly examinations to ensure the disease has not progressed. She credits the experienced team at the Pediatric Retinal and Optic Nerve Center for helping her diagnose and provide highly specialized, ongoing care for complex conditions like FEVR.